This Equity in Action story is distilled from an interview with Amy Stevens and Scott Fry, Advisors on the Health Equity, Partnerships and Innovation Team at Peel Region’s Health Services Department. The interview took place in January 2025, and the details should be considered within the context of that time period.
Peel Region made impactful changes to their public health approach during the COVID-19 pandemic. Recognizing gaps in a one-size-fits-all approach, the Health Services team slowed down, engaged with members of Peel’s diverse communities and co-designed tailored approaches to advance health equity. Witnessing the success of a community-based approach, and not wanting to lose momentum, Peel Region embarked on a journey to embed health equity and human-centredness throughout its health services.
This Equity in Action story is part two of the Peel Region story. To learn more about its community-based approach to the pandemic, please see COVID-19 immunization response in Peel Region: Lessons in humility, relationships and power.
Reflecting on lessons learned during the pandemic
Early on during the COVID-19 pandemic, Peel Region, like many health organizations, was rapidly redeploying staff to respond to the emergency. When vaccines became widely available, our newly formed response team addressed the provincial vaccination mandate in a standard way by opening mass one-size-fits-all vaccination centres.
Many redeployed staff found themselves working directly with people impacted by public health mandates, decisions and programming. It quickly became clear that, because the community of Peel is diverse, one size does not fit all. We did not fully understand people’s lived experiences. This recognition spurred a shift towards more community-based methods, including designing clinics and outreach strategies with our communities.
The success we had with these community-based approaches encouraged our team to reflect more broadly on the ways that our organization approached its work pre-pandemic, through the pandemic and now how we will approach it post-pandemic. We asked ourselves, “How can we best learn from our experiences during the pandemic and evolve the way we work, plan and collaborate?”
What really stuck out in the success of the COVID-19 work was the value of slowing down and prioritizing community partnership for longer-term and more sustainable outcomes. Sustainability is built when health services are flexible, and when we listen to the community and understand their needs. Developing interventions with them as opposed to applying a template allows for tailored programming that better meets the needs of unique communities.
Peel Region’s pandemic response showed us that, in an emergency, we were able to mobilize ourselves and serve our community in the ways that they needed, and in a way that prioritized equity. Yet, once the emergency receded, the pull of the “regular” or “status quo” ways of working was strong. It would have been very easy to quickly lose sight of the work that everyone had been working toward during the pandemic.
As the emergency response wound down, Health Services leaders made it clear — we could not go back to old ways of working. We could not let the momentum evaporate. We needed to intentionally bring the approaches and learnings forward and embed new practices across more and more health programs and services.
Embedding health equity through a new strategy
Our leadership identified that to embed health equity in our work and get people out of their silos, we would need to develop a strategy that spanned across all Health Services departments. Equity would become part of performance reviews and leadership appraisals. Embedding equity into our long-term vision and strategy creates a consistent way of working and solidifies equity as a shared priority across all health services. This represented an important shift and commitment from executive leadership.
The first step in development of this new strategy was to design a process to better understand what it would look like to do this work well and what was needed. We knew that we would need evidence to show that anchoring ourselves in community is the best way forward. There would be a need to build an appreciation of engagement and qualitative research skills in an organization that values quantitative data and analysis. Because of this, a thorough discovery process was conducted which included 45 interviews with people across our leadership team and staff, external experts and community partners.
Some of the foundational questions were: “What is the role of Peel Region — are we stewards of the programming or are we providing some funding and stepping aside?” and “Do we have the right people in the room informing the work, or is it just the folks that we tend to work with more often?”
We received feedback about what worked and what we need to improve when it comes to better understanding community needs and working with community. There were conversations that made people pretty uncomfortable, which we are proud of at the end of the day because we were able to work through that together and hold that tension, creating space for new ideas to emerge. We heard from community partners that the human-centred health equity focus felt productive and made the community feel prioritized.
With this evidence from the discovery process in hand, we began to develop a new health equity strategy. In 2024, we started drafting the vision, goals and key projects and initiatives that we could implement to sustainably anchor health equity approaches moving forward. We knew we would have to innovate to apply the lessons learned from the pandemic.
Driving change within a heavily mandated organization
Despite the success of the pandemic approach and the shared vision to prioritize health equity in the Health Services Department, it wasn’t a straightforward path to shift to newer ways of thinking and working. Health Services is a large, complex and heavily mandated organization driven by standards and mandates which can at times lead to limiting beliefs that “we do what we are required to do within the standards.” We found an overwhelmingly strong desire to slide back into what was comfortable before the pandemic and succumb to the pressures of restarting programs quickly.
When you are trying to drive significant, meaningful and sustainable change, it is critical to follow the organizational culture to a certain extent. To create a department-level shift, we needed to understand how change occurs within the organization and what motivators are needed to nudge the behaviours that are key to shift. An example of this is that there were reservations surrounding qualitative approaches as a form of intelligence and a strong focus on appraised research or evaluative evidence. We also knew there was a lack of acceptance around community engagement and community-told stories as forms of evidence. Because we understood the existing culture, we had taken measures in the discovery process to collect abundant evidence of the impact that occurs when applying both quantitative and qualitative approaches in complement.
This work is very much a process, and in an organization as large as ours, it’s going to take time. However, there are strong signs that teams that are beginning to step into new spaces with communities, make new connections and explore new roles for Peel to play that shifts power dynamics and leads to greater collective impact
Laying the foundation to embed health equity across all Peel services
One of our main areas of focus now is building the tools, abilities and competencies to take more equitable approaches in everything we do, recognizing that more work is needed to support interdepartmental collaboration and work across services that address the social determinants of health more broadly than within Health Services alone.
Enhanced sociodemographic data and community data governance
Our community partners were clear that stronger sociodemographic data is needed to inform our community-based approach. Peel Region needs a strong motivator to collect this kind of data and, with the new health equity strategy, a better understanding of the needs of individuals using and not using our programs and services is critical. We are launching an enhanced data collection approach this year with a focus on improved community data governance in collection, contextualization and use of data. This reflects an ongoing commitment to redistribute power to community and find ways to share information responsibly and meaningfully. This data, combined with qualitative evidence, can inform insights that lead to real change and community-informed action.
Models of engagement
Health Services’ strategy also focuses on developing tools to guide productive engagement with community members so that relationship-building and co-design skills are present across teams, and a consistent approach is used collectively as a department. We are not only pushing for a deeper understanding of the communities we serve but also for community-informed, community-led and co-designed programming. A focus on supporting multiple modes of engagement is key. “Who takes the lead?” is an important question to answer across services. This is a significant change as we are accustomed to taking the lead. When you aren’t leading, it’s often more difficult to figure out your role. New models of engagement refashion this concept so that everybody, including the community, can step in to lead at different points depending on context, lived experiences, skills and expertise. Understanding when Health Services should be taking the lead and when we should play a supporting role is an important part of driving change, including the cultural and behavioural changes needed in how we do our work. During the pandemic, our ideas and ways of working didn’t only come from within, they came from our advisory groups and task forces that included and were centred around community voices. These groups helped us better understand how the community feels when we show up and clarify the work we need to do to rebuild and establish trust with some groups. This work is ongoing and some of these community-based advisory groups remain in place post-pandemic, to lead the way forward in how Peel Region can continue to evolve and improve upon how we show up in more consistent ways and how we can rethink and design new models of engaging and working with diverse communities where change is needed.
Example: Collaborating towards wellness in Black, African, and Caribbean communities
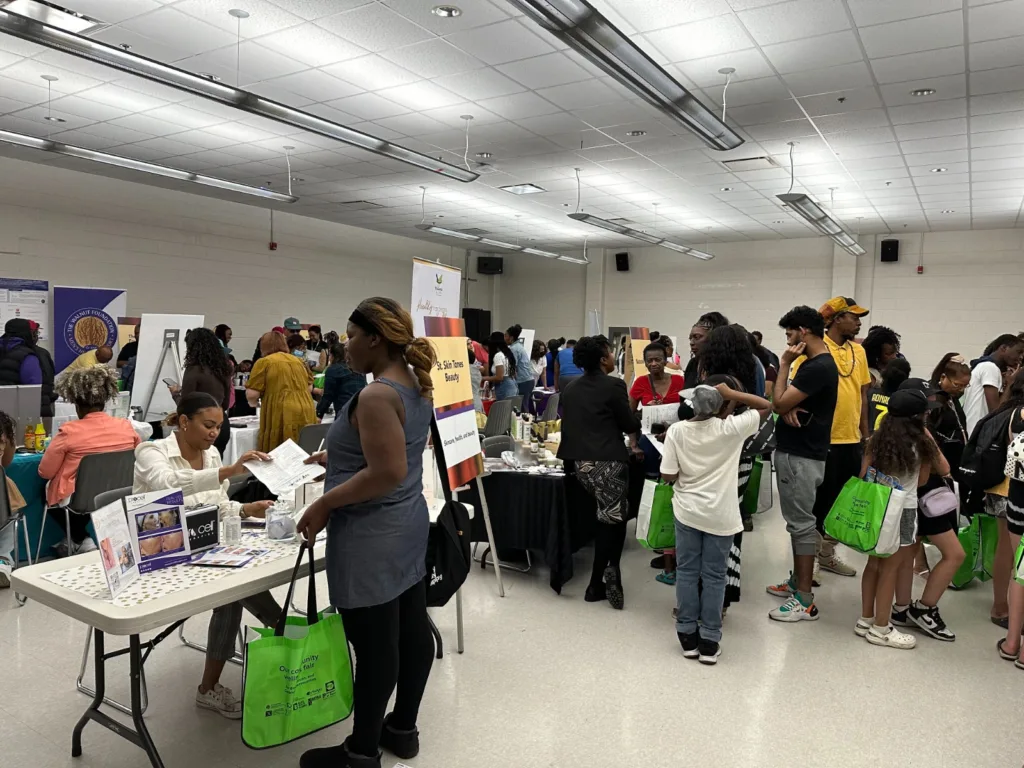
A community collaborative formed during the pandemic to develop holistic wellness initiatives for Peel’s Black, African, and Caribbean communities. Post pandemic, this collaborative is working to reduce inequities experienced by the Black, African, and Caribbean communities by working collaboratively with residents and community partners to increase culturally supportive wellness programming, connection to services, and engagement and social connection. Collaborative initiatives include community-based health fairs and a beauty and barber shop initiative where health professionals showed up in a way that was welcoming and integrated into the community.
Example: Community Safety and Wellbeing Plan
A provincial directive requires municipalities to implement a community safety and wellbeing plan, recognizing that we can’t police our way to community safety and that systems-level collaboration across social determinants is needed. Peel Region is innovating its approach to the plan and moving to a new model of engagement, collective impact and co-design that is centred around deeply understanding community needs, lived experiences and emerging issues, and enabling new ways of working to amplify systems impact including more customizable responses and actions that reflect community-based needs. Part of the evolution of this plan includes Peel Region defining a clearer role to help harness community capacity as a convener of community voices and system partners, providing expertise, innovative processes and stewarding skills to build the collective capacity of the collaborative to drive long-term change and impact together. This work demonstrates Peel’s commitment to new models of engagement that show Peel stepping into new spaces and roles where the community requires us to be.
In both examples, Peel Region is working to demonstrate and embed new mechanisms and models of engagement and truer forms of co-design which move beyond just sharing information with community. These approaches focus on anchoring health equity through cross-sectoral and systems-based action, deepening relationships with community partners and redistributing power and influence where imbalance is present. Work is underway to strengthen recognition of the power imbalances that persist and will require concerted effort over time to shift. Paying closer attention to who comes to the table already and what is preventing people from being at the table and determining what methods are needed to reach these voices is critical. A key mindset shift underscoring this work is about a broader movement where we see ourselves “working with” community rather than “working for” community. In a community as diverse as Peel, we must continue to get closer to our communities, become more proficient in community-based design and engagement, and push for more meaningful models based in deep understanding of community needs and lived experiences to inform and reform how we plan and design equitable and meaningful services and responses.
Ongoing professional development focused on health equity
A third foundational initiative that has surfaced out of this work is developing a core definition of health equity for our organization. Even in the “determinants of health age” of public health, this is still a big learning curve for staff. We are building a staff learning system that focuses on education about health equity and what it means for our workforce and how we work to advance health equity within the system in which we exist. This education is also built into our Health Services Strategy to become a learning organization that continually reinvents itself and its ways of working to reflect the evolving needs of our diverse community.
Identifying facilitators and barriers to collective organizational change
You can’t underestimate the role of leadership in supporting new behaviour and mindset changes. Every bureaucratic organization faces resistance to change and can fall back on the comfort of doing what we have always done. We got stuck many times in organizational process and culture. Even with a shared desire internally to work differently, it was still very hard to shift thinking and ways of working within a complex and heavily mandated organization. The consistent and strong commitment from senior leadership who had internalized the learnings from the COVID-19 response kept the necessary tension between what we wanted to move towards and where we were at. This was one of the most valuable roles for leadership to play – to resist the natural human desire to revert to what we know and where we are most comfortable. This showed that health equity is not just a buzz word but a long-term commitment to go where the community needs us to be and reimagine the roles we must play in newer and unfamiliar spaces.
The relationships built during COVID-19 pandemic have opened avenues for broader and more constructive dialogues to emerge. The impact of this is that we are beginning to shift power dynamics and create space for deeper insights from the community to point us to where we still have gaps, like in the case of our approach to collecting sociodemographic data. Trust is built over time and enables a more authentic understanding of strengths and weaknesses, as well as facilitators and barriers, leading to positive growth and change.
Seeing the impact of an organizational commitment to health equity
Stepping into new spaces with piloted initiatives and new ways of engaging community members has started to change conversations within our organization and with our community. We have heard from our community partners that they see and feel our commitment to authentic partnership. This collaborative way of working is leading to programming that is more aligned with what community needs. Intentionally sharing learnings and insights from this work helps inform systems-wide change, supporting improvements to service design and delivery across sectors.
The impact of this work is also starting to change the expectation that funding agencies have when investing in community-based work. An example of this are the health fairs in the Black, African and Caribbean communities of Peel Region. This collaboration with the Black, African and Caribbean communities is a great example because this project was not part of our mandated work, we don’t have a mandate to be there, but it showed Peel Region that working more flexibly, showing up where we are welcome and slowing down to listen to communities opens new avenues and opportunities. The learnings from the fairs and the larger collaborative were formative to achieving a large funding opportunity to form a Black health and social services hub in Peel. This Hub, created and operated by community health and social services agencies, will provide culturally relevant health and social services in a supportive environment.
Moving forward, we are excited to continue exploring how we can generate new ways of working that build competencies and capacity to support approaches that improve health equity and community engagement and shift power dynamics. It is a long process, but we continue to push within our organizational structure to create movement, address power constructs and serve our communities in ways that address their needs and experiences.
Lessons learned

We need to intentionally sit in the discomfort of creative tension. Health Services continues to learn how to better work within broader systems and structures to drive change, but there is a tendency to go back to what’s comfortable and what we’ve done before. The role of leadership to resist this tendency and hold creative tension is key.

Organization-level shifts take time. To spark change, one must understand the organizational culture and work within it, not against it.

Large-scale change does not happen without individual change. It is important to create an imperative inside the organization for individual accountability and responsibility to learn and grow.
Background
Region of Peel delivers essential social, health, and public works services to 1.5 million residents and over 175,000 businesses in Brampton, Caledon and Mississauga, Ontario. Peel is highly diverse with 69% of the population identifying in 2023 with a racialized group (compared to 34% of Ontarians). Peel’s racialized population has increased by 72% since 2006, and 52% of Peel’s residents are immigrants.
More demographic info can be found here.
Resources
Getting to the heart of health equity at Peel: Discovery Phase findings report (2023)
To learn more about the initiative described in this story, contact the National Collaborating Centre for Determinants of Health, at nccdh@stfx.ca.
Do you have an idea for an Equity in Action story? If you have heard of other health equity-promoting initiatives in Canada that we should share, please let us know.